I am a firm believer that stories reveal more truths than statistics. Yet when I first dove deep into the world of Mental Health Research, I noticed a pattern. Borderline Personality Disorder in men is frequently misdiagnosed. As a psychiatrist and a critical observer, I have seen the confusion, mislabeling, and the heartbreak that follows.
I still remember the first time I sat across from a male patient who, beneath the layers of anger and indifference, was quietly falling apart. He wasn’t loud about his suffering; he joked through it. Humor, you know. It’s a mature defense mechanism to cope with stress. He turned every heartbreak into sarcasm, every tear into a smirk. On paper, he was aggressive, impulsive, and even antisocial. I didn’t follow what was written on the paper. Instead, I chose to listen to the painful cries as he spoke. I could feel it, that raw, trembling ache that screamed abandonment, emptiness, and fear.
Borderline Personality Disorder in men often hides behind labels that feel “more masculine” or safer. Society allows men to express rage, but not weep; to break things, but not admit they are broken. Therefore, many of them are misread, not just by the world, but also by the very professionals meant to understand them.
So today, I wish to peel back the curtain on this quiet epidemic, the systemic misdiagnosis of Borderline Personality Disorder in men. Not from the sterile tone of a textbook, but from the lens of someone who has seen it up close, wrestled with its complexity, and asked the haunting question: “What if we have been mislabeling their pain all along?”
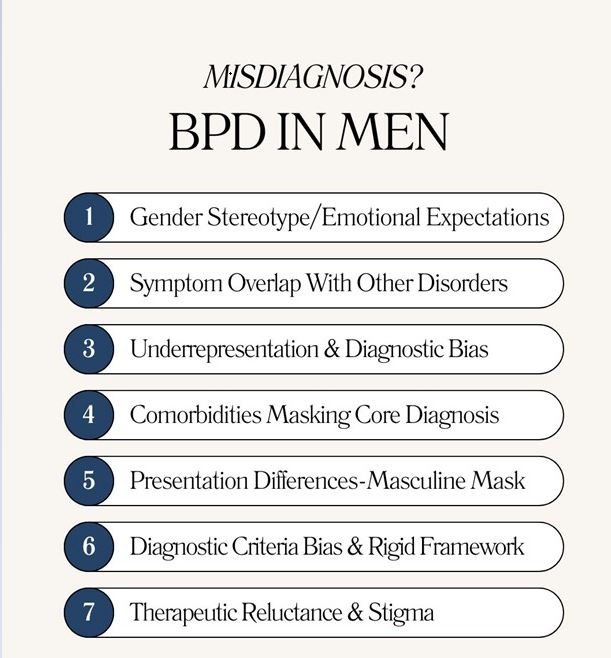
1. Gender Stereotypes & Emotional Expectation.
From early on, many cultures, especially South-Asian cultures, teach boys not to cry, not to express how they feel, and to be strong. It is considered a sign of weakness if a man dares to even shed a single tear. So when an emotionally volatile man, with an identity crisis or chronic emptiness, seeks help, his symptoms are reframed as aggression, substance abuse, or antisocial behavior. The emotional expressions of borderline personality disorder in men may be silent, distorted, or externalized in dangerous ways, while women tend to turn that turmoil inward through self-harm or visible emotional dysregulation. Hence, clinicians get confused and interpret them through a “male” perspective of anger or defiance.
The reality is that men with BPD feel as deeply as women; they just carry their pain differently. One of my patients once said something, and it struck with me, “I don’t cry rivers; I flood cities from underground”.
2. Symptoms Overlap with Other Disorders.
If I could rename Psychiatric overlap, I’d call it “Diagnostic Dejavu”. Borderline Personality Disorder in men shares symptoms with Mood Disorders, Antisocial Personality Disorder, PTSD, and substance use disorders, and that’s where the chaos begins.
Men with BPD are often wrongly diagnosed with:
- Bipolar Disorder: Due to mood swings and impulsivity.
- Antisocial Personality Disorder: Due to aggression or disregard for rules.
- Substance Use Disorder: Because many men self-medicate to cope with anxiety associated with emotional instability.
According to the National Alliance on Mental Illness (NAMI), around 40% of individuals who meet the criteria for BPD have previously been labeled as having Bipolar Disorder. That’s a staggering overlap-and a heartbreaking one, considering how different the therapeutic approaches are.
3. Underrepresentation & Diagnostic Bias.
Do you know what is ironic? Despite data showing nearly equal prevalence across genders, borderline personality disorder in men is still viewed as “rare”. Why? That’s because clinical studies, case reports, and even diagnostic training examples are disproportionately based on female presentations.
The outcome? Diagnostic bias. A man who fits the criteria of BPD might instead be tagged as “Antisocial”, simply because his emotional expression aligns less with the conventional BPD portrait.
A wide range of research from the American Psychological Association shows that men’s BPD symptoms are often mislabeled, reflecting the unconscious bias that “Borderline” equals “Women”. This misunderstanding runs deep, right into the Psychotherapy sessions.
“Bias is the invisible ink that rewrites the stories we think we’re reading correctly.”
4. Comorbidities Masking the Core Disorder.
One of the trickiest aspects of borderline personality disorder in men is how often it coexists with other mental health conditions.
A fact to remember: Substance Use Disorder, Depression, Anxiety, and PTSD aren’t just comorbid; they are often the first things clinicians take notes of.
A man who drinks or smokes excessively to numb his emptiness gets labeled as an “Alcoholic/Substance Abuser”. The one who feels lost and hollow might be told he has “Depressive Disorder”. The one who lashed out when abandoned gets called “Impulsive/Aggressive”. And yet, all these are fragments of a deeper core, an unstable self that fits the criteria of BPD perfectly.
It’s exactly like treating smoke while ignoring the fire.
5. Presentation Differences “Masculine Mask”.
If I had a dollar for every man who told me, “I am fine”, right after describing a storm of chaos, I’d fund a campaign for emotional honesty.
Men with BPD often wear a mask of confidence, humor, or indifference to protect their fragile inner selves from worldly judgment and criticism. Behind this facade lies an overwhelming fear of abandonment and identity confusion. They hardly ever admit feeling “emotionally disturbed” because of rejection. Hence, they present as agitated, reckless, or detached.
One of my favorite quotes about this dynamic goes:
“Some men wear strength like armor, not realizing it’s made of glass”.
This masking makes it difficult to establish an accurate diagnosis. Because clinicians see the armor, not the cracks, borderline personality disorder in men remains hidden beneath the illusion of control.
6. Diagnostic Criteria Bias & Rigid Frameworks.
The Diagnostic and Statistical Manual of Mental Disorders (DSM), though a valuable tool, wasn’t built in a cultural vacuum. Its historical data and case patterns are heavily skewed toward BPD presentations, i.e, Deliberate self-harm, Mood swings, Dependency, and Attachment issues.
But men? They often demonstrate similar pathology but in different ways, such as aggression, substance abuse, or risky sexual behavior. The foundation is the same, costume is different. Since the diagnostic criteria are rigid, the presentation of borderline personality disorder in men doesn’t always “tick enough boxes”.
A male colleague joked with me once, “If the DSM were a GPS, it would reroute the moment a man who shows up angry instead of tearful”. We laughed, but deep down, both of us knew it was a bitter truth that hurt.
7. Therapeutic Reluctance & Stigma.
Even when Psychiatrists suspect borderline personality disorder in men, many people hesitate to use the label. The stigma revolving around BPD is real. It is often viewed as “Manipulative”, “Draining”, or “Untreatable”. When the patient is a male, the stigma amplifies; the label feels much heavier.
Some Psychotherapists unconsciously choose “safer” diagnoses such as Depression or Substance Abuse. Meanwhile, most men themselves reject the idea of having a “Personality Disorder”, substituting it with being “Damaged’.
But here is the paradox: Correct labeling opens doors to proper management. Avoiding the terminology only keeps individuals trapped in cycles of misdirected treatment.
What Does This All Mean & What Is My Learning?
When we look back, we see that borderline personality disorder in men is misdiagnosed for reasons that are both structural and human: Bias in training, rigid diagnostic criteria, masking of symptoms by patients, and overlapping signs. But I’ll be straightforward here: Misdiagnosis costs lives. Men with untreated BPD often struggle with repeated self-harm, substance abuse, chronic despair, or incarceration. The worst part is, it is reflected in their day-to-day affairs.
But here is the hopeful counterpart: With awareness, training, and curiosity, clinicians and loved ones can detect the deeper patterns. I genuinely believe we need:
- More gender-specific diagnostic tools.
- Training to look beyond superficial expressions.
- Integration of Trauma, Personality, and Behavioral Approaches.
- Therapies like Dialectical Behavioral Therapy (DBT), Cognitive Behavioral Therapy (CBT), Mentalization-Based Therapy (MBT), and others applied without gender prejudice.
Jokes apart, diagnosing someone’s inner landscape is like being given a map to buried treasure, but only if you are dedicated enough to dig deeper and not judge by the weeds.
FAQs
1. Can men with BPD improve or recover?
Yes, for sure. Therapies such as DBT, MBT, and Schema Therapy have shown benefit. Recovery is not a “cure,” but learning new ways to regulate emotions, rebuild relationships, and reduce self-harm.
2. What symptoms in men hint at BPD (other than Substance Abuse)?
Look for identity crisis, fear of abandonment (even if masked), chronic emptiness, intense & unstable relationships, and emotional reactivity behind outward displays.
3. How can loved ones support a man who may have BPD?
Listen to them without judgment, avoid blame, validate emotional pain, create boundaries, and encourage them to seek professional help. Try gathering information from reputable resources such as NAMI or DBT workbook material.
4. What’s one sign clinicians should never overlook?
When anger feels disproportionate to the trigger, that’s often fear disguised as fury. Look deeper!
5. When should one seek a specialist’s help?
If repeated diagnoses of Bipolar Disorder, Depression, Substance Abuse, or personality “not other specified” fail to explain the pattern, especially when emotional instability or impulsivity is constant, seek clinicians trained in Personality Disorders or DBT.
In Closing
I may not carry all the final answers, but I definitely carry a conviction: Borderline Personality Disorder in men deserves fuller recognition, deeper curiosity, and compassionate diagnosis. Misdiagnosis isn’t just a sterile clinical error; it is an erasure of struggle, a denial of inner life.
Let’s walk forward with humility and curiosity. Let us listen for the anxiousness beneath the facade. And let’s believe that men’s emotional lives, even when stormy, deserve care and affection instead of judgment.
If you see any of your loved ones suffering from supposed anger issues or emotional instability, feel free to reach out to us at Youth Table Talk. Help them get the help they deserve.
Dr. Talia Siddiq is a resident psychiatrist in training at Dr. Ruth K.M. Pfau Civil Hospital Karachi, deeply passionate about understanding the human mind and helping people find healing. Beyond her clinical work, she is also a writer who believes that mental health conversations should be easy, relatable, and stigma-free.
She started writing in 2020, turning her reflections and experiences into articles that speak to the struggles many young people silently face—whether it’s self-harm, addictions, relationships, or simply finding direction in life. Over time, her writing has expanded into areas like career guidance and financial independence, because she strongly believes that resilience isn’t just about surviving emotionally—it’s about building a meaningful, balanced life.
For Talia, YouthTableTalk is more than a blog. It’s a safe corner on the internet where young people can pause, reflect, and feel understood. Her goal is not to lecture but to have a conversation—just like a friend who listens, shares, and gently guides you toward growth.
When she isn’t studying psychiatry or writing, you’ll often find her reading, exploring self-growth books, or cooking something new for her family. She brings the same curiosity and compassion to her personal life that she does to her work: always seeking better ways to connect, learn, and inspire.
Through YouthTableTalk, she hopes to remind every reader of one simple truth: you’re not alone, and your story matters.
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/