Hello, my dear readers,
Welcome to Youth Table Talk once again!
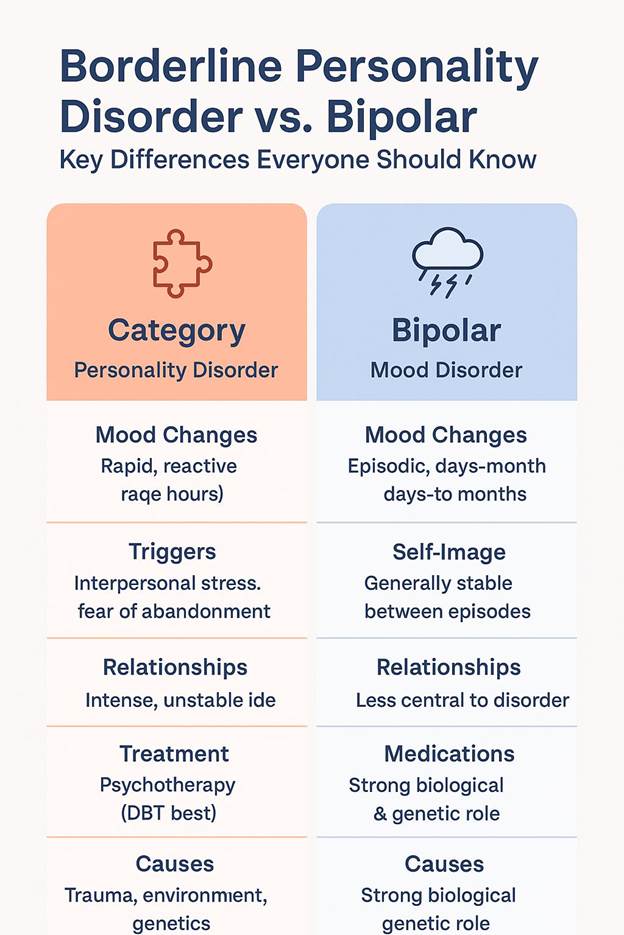
When I first stepped into the world of Psychiatry residency, I was confused about so many phenomena. Most of the concepts seemed as strange as mathematical algorithms. One such concept was borderline personality disorder vs bipolar disorder. Both disorders share a constellation of symptoms, but the major one is rapid “mood swings”. However, these two disorders are polar apart when you peel away the layers of signs, symptoms, causes, and management plans.
As Carl Jung wisely said, “The shoe that fits one person pinches another; there is no recipe for living that suits all cases.” Similarly, no single label of a disorder can capture the uniqueness of one’s struggles in the true essence. That’s why I feel so passionate about helping you delineate between borderline personality disorder vs bipolar disorder. Coming with this detailing directly from a psychiatrist helps build trust and clears any form of misunderstanding.
Why do Individuals Get Confused?
I have observed that the general public and sometimes even the patients struggle to separate these two conditions. Well, the reason is simple: both involve mood shifts, emotional instability, and difficulties in relationships. But here is the key idea:
Borderline Personality Disorder is a personality disorder, whereas Bipolar Disorder is essentially a mood disorder. This fundamental difference changes everything from presenting complaints to management.
I like to think of it this way: Bipolar Disorder is like the weather (storms come and go), while BPD is like the climate (the overall atmosphere that paints life every single day).
Figuring out borderline personality disorder (BPD)
When I explain BPD to my patients or students, I describe it as living life on an emotional rollercoaster, without a seatbelt. Individuals suffering from BPD often feel emotions at an intensity and frequency that others can’t even imagine.
Symptoms of BPD:
- Extreme fear of rejection and abandonment, whether real or imagined.
- Unstable relationships fluctuating between idealization and devaluation (similar to Narcissistic Personality Disorder)
- A fragile or shifting sense of self, i.e, distorted self-image.
- Rapid mood changes are often triggered by interpersonal stress.
- Highly impulsive behavior (reckless spending, overspeeding, unsafe sex, substance abuse)
- Persistent feelings of emptiness
- Recurrent self-harm or suicidal thoughts.
- Intense anger or difficulty controlling it.
I remember a patient with BPD once reported to me, “It feels like my emotions are firecrackers—tiny sparks set me off, and I explode before I can think.”
Visit NIMH for clarity and a better understanding.
Cracking the Code of Bipolar Disorder
As opposed to BPD, Bipolar Disorder does not involve everyday emotional chaos. It’s more like episodes- a distinct period of mood elevation (also known as mania or hypomania) and depression that may last from a few days to weeks to even months.
Symptoms of Bipolar Disorder-Mania/Hypomania
- Elated mood, irritability, or expansiveness
- Emotional lability
- Increased energy
- Decreased need for sleep
- Rapid speech
- Racing thoughts (Flight of ideas)
- Risky behaviors (Overspending, unprotected sexual activities, multiple partners, reckless driving)
- Aggressive outbursts
Symptoms of Bipolar Disorder-Depression
- Persistent low mood, sadness, and feelings of emptiness
- Loss of interest in activities
- Fatigue
- Poor concentration
- Feelings of guilt
- Worthlessness
- Suicidal ideation
The noteworthy point over here is that BPD emotions can fluctuate with hours, while Bipolar mood swings occur across days or weeks. If you want to discover deeper depths of Bipolar Disorder, visit NIMH.
Causes: Borderline Personality Disorder VS Bipolar Disorder
- BPD: Most frequently linked with childhood adversities, trauma, a history of abuse, attachment issues with the primary caregiver, genetic vulnerability, and environmental stressors. Patients often give accounts of sexual violence and parental neglect.
- Bipolar Disorder: A very strong genetic and biological component. Research shows that the heritability factor of Bipolar Disorder is approximately 85%. Family history also plays a significant role, along with the interplay of neurotransmitters and chemical imbalances.
Treatment Approaches
This is the true point of divergence, I would say. Let me walk you down the road of management plans for both disorders separately.
- BPD: Psychotherapy remains the mainstay of treatment here. The two major types of therapies used in BPD are Dialectical Behavior Therapy (DBT) and Cognitive Behavior Therapy (CBT). Medication such as Anti-Depressants can help with co-occurring Anxiety, Depression, etc.
- Bipolar Disorder: Drugs remain the cornerstone of bipolar disorder. Mood stabilizers (such as Lithium, Sodium Valproate), Antipsychotics, and sometimes Anti-Depressants are of most help. Psychotherapy is important, but alone it’s of no use.
Why Is It Crucial to Know the Difference?
I cannot emphasize enough on the need to have an accurate diagnosis. Incorrectly labeling someone can cause a delay in the right treatment and enhance their suffering in a way that even I, as a psychiatrist, can’t imagine. Correct diagnosis can literally change the trajectory of someone’s life.
For example, imagine a person with BPD who is wrongly treated for bipolar disorder. Just because of a misdiagnosis, the whole management line changes. The patient with BPD might be prescribed Mood Stabilizers or Antipsychotics. Can you even imagine what these so powerful and heavy drugs do to that poor individual? Their adverse side effect profile can literally leave that otherwise normal individual more confused and anxious than ever. The least possible help that these medications provide is dulling the emotional reactivity of a patient with BPD, nothing else. The real healing comes from Psychotherapy, predominantly DBT. Without therapy, individuals with BPD continue to suffer from self-harm, risk-taking behavior, feelings of emptiness, and painful relationships, wondering why medication is not working.
Now imagine the opposite: A person with bipolar disorder being told that they just need Psychotherapy for relationship instability or emotional dysregulation. Psychotherapy can help with these issues somewhat, but it cannot help manage the “extreme highs” and “crushing lows” that are a core feature of bipolar disorder. Therefore, the primary way to deal with these mood episodes is to take medication, as I mentioned above. Without the right type of medication, the person risks sliding into severe depression or switching into mania that could jeopardize their finances, relationships, or even their safety.
This is why understanding borderline personality disorder vs bipolar disorder is so essential. Currently, I am sitting in my Outpatient Department as I write this article. When I sit with my patients, I remind myself: every correct diagnosis is like handing the right roadmap to my patients. With the wrong guidance, they will keep walking in circles, fatigued and lost. With the right one, they will feel worried initially and may face challenges, but at least they will know where they are headed and how to prepare for the journey.
A renowned Psychiatrist, Karl Menninger, once said, “What the patient does not say is often more important than what he does say”. Paying close attention, asking the right questions, and clarifying borderline personality disorder vs bipolar disorder ensures that what remains unsaid doesn’t become an overlooked suffering.
My Personal Reflection
As a resident psychiatrist, I have seen individuals with both sorts of disorders. And I can safely say that these individuals are not as dangerous or unstable as society labels them. They are warriors and survivors of the silent battles, carrying wounds that run so deep. Their courage to seek professional help humbles me to the core.
After several months of therapy, a patient with BPD told me, “For the first time in my life, I feel like I have tools instead of weapons against myself”. This statement was enough to convince me of the profound effect that correct diagnosis and treatment can have.
FAQs About Borderline Personality Disorder vs bipolar disorder
1. Can someone have a dual diagnosis of BPD as well as bipolar disorder?
Yes, it is quite possible. However, careful evaluation is needed to differentiate between overlapping symptoms. There is also a high chance that individuals with BPD develop bipolar disorder later in life and vice versa.
2. Which of the two conditions is more common?
BPD affects around 1.6% of the population, while Bipolar affects about 2.8%. Both conditions are relatively common.
3. Are mood swings in BPD the same as in bipolar disorder?
No. Not at all. Mood swings in BPD are short-lived and triggered by events, or interpersonal conflicts, etc. Whereas the Bipolar mood episodes can last days to months and may not need triggers. However, lack of sleep or a disturbed routine seems to have a significant impact on the triggering of an episode.
4. Can only medication cure BPD?
No. Like I said earlier, medication can only help with the co-occurring Anxiety/Depression, but the mainstay of the treatment remains Psychotherapy (DBT, CBT).
5. Is Bipolar Disorder Inherited?
Yes, actually. Bipolar Disorder is multifactorial, but genetics play a major role (85%). Having a first-degree relative with bipolar disorder significantly increases the risk of an individual having it.
6. Can people with either disorder live meaningful lives?
Sure, why not? If diagnosed timely and correctly, patients can initiate their treatment plan. With proper diagnosis, treatment, and psychosocial support, individuals can lead stable, successful, and fulfilling lives.
References:
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition (DSM-5).
- National Institute of Mental Health. Bipolar Disorder.
- National Institute of Mental Health. Borderline Personality Disorder.
- Linehan, M. M. (1993). Cognitive-Behavioral Treatment of Borderline Personality Disorder.
Dr. Talia Siddiq is a resident psychiatrist in training at Dr. Ruth K.M. Pfau Civil Hospital Karachi, deeply passionate about understanding the human mind and helping people find healing. Beyond her clinical work, she is also a writer who believes that mental health conversations should be easy, relatable, and stigma-free.
She started writing in 2020, turning her reflections and experiences into articles that speak to the struggles many young people silently face—whether it’s self-harm, addictions, relationships, or simply finding direction in life. Over time, her writing has expanded into areas like career guidance and financial independence, because she strongly believes that resilience isn’t just about surviving emotionally—it’s about building a meaningful, balanced life.
For Talia, YouthTableTalk is more than a blog. It’s a safe corner on the internet where young people can pause, reflect, and feel understood. Her goal is not to lecture but to have a conversation—just like a friend who listens, shares, and gently guides you toward growth.
When she isn’t studying psychiatry or writing, you’ll often find her reading, exploring self-growth books, or cooking something new for her family. She brings the same curiosity and compassion to her personal life that she does to her work: always seeking better ways to connect, learn, and inspire.
Through YouthTableTalk, she hopes to remind every reader of one simple truth: you’re not alone, and your story matters.

