“OCD is not about being neat. It is about being afraid—deeply, persistently, and often silently.”
My dear readers,
As a psychiatrist, I often encounter people who come to me saying, “I think too much, and I can’t resist my thoughts”. If you get to the bottom of it, what they are describing is Obsessive-Compulsive Disorder (OCD) slowly tightening its grip on their inner world.
What I am writing today is a sort of sequel to my previous article, where we briefly discussed the types of OCD, more like an introductory guide. Today, I would like to invite you all to explore OCD more deeply from a clinical and scientific perspective.
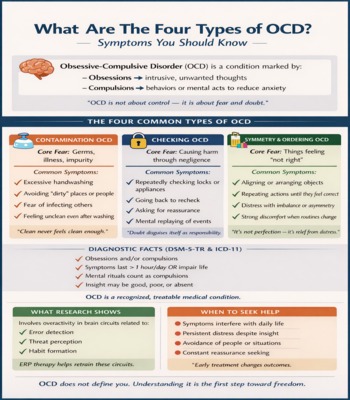
Here, I will take you through What Are The Four Types Of OCD, focusing on Symptoms You Should Know, while grounding everything in DSM-5-TR and ICD-11 diagnostic frameworks, real clinical experience, and current research.
OCD: More Than Habits, More Than Anxiety
OCD is often trivialized as being “too clean” or “too organized”. In reality, it is a disorder of pathological doubt and misfiring threat perception.
At its core, OCD consists of:
- Obsessions: Repeated, intrusive, unwanted thoughts, urges, or images.
- Compulsions: Repetitive behaviors or mental acts aimed at reducing distress.
What makes OCD uniquely painful is that insight often remains intact-the person knows the fear is irrational, yet feels unable to stop responding to it.
DSM-5-TR Diagnostic Criteria For OCD (Clinically Explained)
From a psychiatric point of view and according to the DSM-5-TR (Diagnostic Statistic Manual-5-TR), OCD is diagnosed when the following criteria are met:
Criteria A: Obsessions, Compulsions, or Both
Obsessions are:
- Recurrent and persistent thoughts, urges, or images.
- Experienced as intrusive and unwanted.
- Causing marked anxiety or distress.
- Actively resisted or neutralized.
Compulsions are:
- Repetitive behaviors (washing, checking, ordering).
- Or mental acts (counting, praying, reviewing).
- Performed in response to obsessions.
- Aimed at reducing distress or preventing feared outcomes.
- Not realistically connected to the feared event.
In my clinical practice, many patients are surprised to learn that mental rituals count as compulsions.
Criterion B: Time-Consuming or Distressing
- Symptoms take more than one hour per day,
OR
- Cause significant impairment in daily functioning
This criterion separates OCD from everyday worries or personality traits.
Criteria C & D
Symptoms are:
- Not to do psychoactive substance use or any other medical condition.
- Not better explained by another mental health condition.
You can check out the American Psychiatric Association for more in-depth learning.
ICD-11 Perspective: A Global View Of OCD
The ICD-11 aligns closely with DSM-5-TR but emphasizes:
- Variable levels of insight.
- Mental compulsions and avoidance.
- Functional impairment over rigid symptom counts.
The ICD-11 recognizes OCD as a spectrum disorder, which accurately reflects what I see clinically, symptoms shift, evolve, and overlap.
Feel free to check out the ICD-11 by the WHO.
What Are The 4 Types Of OCD? (Symptom-Focused Classification)
These are the phenomenological subtypes, not official diagnoses-but they are extremely helpful in understanding symptom patterns.
1. When Safety Never Feels Certain: Contamination OCD
“Clean is not a destination—it is a moving target.”
Principle Obsessions
- Fear of germs, dirt, bodily fluids, chemicals, or moral contamination.
Common Symptoms
- Fear of contaminating others.
- Excessive handwashing or showering.
- Persistent doubt even after cleaning.
- Avoidance of public places or shared objects.
A lesser-known symptom is mental contamination, i.e, feeling dirty after having certain thoughts or interactions rather than physical contact.
2. Doubt Disguised As Responsibility: Checking OCD
“OCD weaponizes conscience.”
Principle Obsessions
- Fear of causing harm through negligence.
Symptoms I commonly observe
- Repeated checking of door locks, appliances, switches, and gas knobs.
- Returning home multiple times.
- Mental replaying of events.
- Excessive seeking of reassurance.
Checking paradoxically strengthens doubt, reinforcing the OCD cycle.
3. The Tyranny Of Getting Things “Just Right”: Symmetry & Ordering OCD
“It’s not about beauty—it’s about relief.”
Principle Obsessions
- Distress related to asymmetry, imbalance, and incompleteness.
Symptoms
- Aligning/lining up objects.
- Repeating actions until they feel correct.
- Body-focused symmetry sensations.
- Intense discomfort when routines are disturbed.
This subtype is often mistaken for perfectionism. The difference is crucial: perfectionism seeks excellence; OCD seeks relief from distress.
4. The Quietest, Loudest Suffering: Intrusive Thoughts (Pure O)
“The mind becomes a courtroom where every thought is evidence.”
Principle Obsessions
- Violent, sexual, religious, or morally unacceptable thoughts.
Common Themes
- Sexual intrusive imagery.
- Blasphemous or taboo thoughts.
- Fear of harming loved ones.
- Fear of being immoral or dangerous.
Mental Compulsions
- Silent prayers.
- Thought suppression.
- Mental reassurance.
- Thought suppression.
Let me say this clearly, as I tell my patients:
Intrusive thoughts are not intentions. They are symptoms.
For compassionate discussions that normalize such experiences, platforms like Youth Table Talk play an important role in mental-health literacy.
What Research Tells Us: Neurobiology Of OCD
“OCD is not a failure of willpower—it is a miscommunication between brain circuits designed to protect us.”
The most consistently implicated system is the Cortico-Striato-Thalamo-Cortical (CSTC) Loop. In simple terms, this circuit helps the brain decide:
- Is something wrong?
- Do I need to act?
- Can I stop acting now?
In OCD, this loop becomes overactive and poorly regulated.
Key brain regions involved include:
- Orbitofrontal Cortex
Responsible for evaluating danger and assigning significance. In OCD, it sends excessive “something is wrong” signals, even when no real threat exists.
- Anterior Cingulate Cortex
It plays a major role in error detection and emotional distress. Hyperactivity here explains the constant feeling that something is incomplete or incorrect.
- Basal Ganglia (Cuadate Nucleus)
Involved in habit formation and action selection. Dysfunction here makes it difficult to shift gears or stop repetitive behaviors.
Functional MRI studies repeatedly show hyperactivity in these regions, particularly during symptom provocation.
Why Do Compulsions Provide Temporary Relief?
One of the most misunderstood aspects of OCD is why compulsions feel so urgent and necessary.
From a neurobiological standpoint:
- Compulsions temporarily dampen hyperactivity in the CSTC circuit.
- This creates short-term relief.
- The brain then learns that the compulsion “worked”.
This reinforcement loop strengthens over time, not because the person wants it to, but because the brain is responding to the perceived threat.
Neuroplasticity & Treatment
The hopeful part of this entire mental health disorder is Neuroplasticity. It is the brain’s ability to rewire itself.
Research shows that Exposure and Response Prevention (ERP):
- Reduces hyperactivity in the Orbitofrontal Cortex and Anterior Cingulate Cortex.
- Weakens the compulsive habit loop.
- Restores inhibitory control in the Basal Ganglia.
In other words, therapy does not just change thoughts; it changes brain function.
This is why OCD should never be dismissed as “overthinking”. It is a treatable neuropsychiatric condition with appropriate biological correlates.
When To Seek Professional Help For OCD?
“The right time to seek help is not when symptoms become unbearable—it is when they begin to shrink your life.”
Many People delay seeking treatment because:
- They feel embarrassed due to their obsessions.
- They fear being judged or misunderstood.
- They recognize their thoughts as irrational.
As a psychiatrist, I want to clarify this: having insight doesn’t protect you from suffering.
You should consider seeking professional help if any of the following apply:
1. Symptoms are time-consuming.
If obsessions or compulsions take more than an hour per day, or if they repeatedly interrupt your daily activities.
2. You feel persistent distress or mental exhaustion.
Even without evident rituals, constant rumination, mental checking, and thought suppression can lead to emotional burnout, sleep disturbance, and depressive symptoms.
3. Avoidance is increasing.
Avoidance is a silent marker of worsening OCD:
- Avoiding people, places, or responsibilities.
- Structuring life around “triggers”.
- Shrinking social or professional engagement.
Avoidance may feel protective, but it strengthens fear long-term.
4. Reassurance seeking is becoming a pattern.
If you find yourself repeatedly:
- Asking others to confirm safety.
- Seeking online reassurance.
- Mentally reviewing decisions.
This indicates OCD is the driving behavior, even if insight is present.
5. Symptoms are shifting, not disappearing.
A common misconception is:
“At least it’s not as bad as before.”
In reality, OCD often changes themes-from contamination to harm, from checking to intrusive thoughts-while the core disorder persists.
6. You are unsure whether medication or therapy is needed.
A trained mental health expert can help determine:
- Whether ERP alone is sufficient.
- Whether medication may be helpful or not.
- How to tailor treatment to symptom subtype and insight level.
Early intervention improves outcomes significantly.
FAQs
1. Can someone have all four types of OCD at the same time?
Yes. Most individuals experience overlapping symptom dimensions, not a single “pure” subtype. The dominant theme may change over time, especially under stress.
2. Are intrusive thoughts an indication that I might act on them?
No. Research consistently shows that intrusive thoughts in OCD are ego-dystonic. They go against a person’s values and intentions. They are not predictors of behavior.
3. How is OCD different from Generalized Anxiety Disorder?
In OCD, anxiety is driven by specific intrusive thoughts and relieved through compulsions. In GAD, worry is more diffuse, future-oriented, and not linked to ritualized behaviors.
4. Does having insight mean that the disorder is mild?
No. A lot of patients with excellent insight suffer intensely. Insight reflects awareness, not severity.
5. Can teens and adolescents develop OCD?
Yes. OCD commonly begins in childhood or adolescence, and early treatment can significantly improve the outcomes.
References
- American Psychiatric Association. DSM-5-TR
- World Health Organization. ICD-11
- Stein DJ et al. The neurobiology of OCD. The Lancet Psychiatry
- International OCD Foundation
- National Institute of Mental Health
Dr. Talia Siddiq is a resident psychiatrist in training at Dr. Ruth K.M. Pfau Civil Hospital Karachi, deeply passionate about understanding the human mind and helping people find healing. Beyond her clinical work, she is also a writer who believes that mental health conversations should be easy, relatable, and stigma-free.
She started writing in 2020, turning her reflections and experiences into articles that speak to the struggles many young people silently face—whether it’s self-harm, addictions, relationships, or simply finding direction in life. Over time, her writing has expanded into areas like career guidance and financial independence, because she strongly believes that resilience isn’t just about surviving emotionally—it’s about building a meaningful, balanced life.
For Talia, YouthTableTalk is more than a blog. It’s a safe corner on the internet where young people can pause, reflect, and feel understood. Her goal is not to lecture but to have a conversation—just like a friend who listens, shares, and gently guides you toward growth.
When she isn’t studying psychiatry or writing, you’ll often find her reading, exploring self-growth books, or cooking something new for her family. She brings the same curiosity and compassion to her personal life that she does to her work: always seeking better ways to connect, learn, and inspire.
Through YouthTableTalk, she hopes to remind every reader of one simple truth: you’re not alone, and your story matters.
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/
- Talia siddiqhttps://www.youthtabletalk.com/author/talia-admin/